Twice Daily
Twice Daily
Use your Exergen TemporalScanner Twice Daily at home. The best way to catch a fever. Here's what you need to know.
Twice Daily Temperature Checks at Home
In these times of COVID-19, checking for fever in the morning is not the most accurate time to detect a fever. Our daily circadian rhythm regulates our body temperature, which is lowest in the morning, and highest in the evening. New research shows this happens with fevers as well.
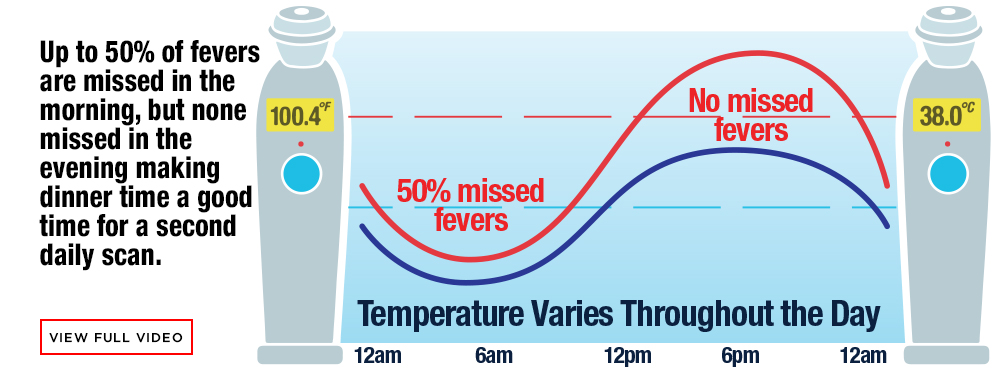
Up to 50% of fevers are missed in the morning, but none are missed in the evening due to circadian effects, making dinner time a good time for a second daily scan. Twice daily morning and evening fever detection is the best defense at home.
Questions and answers below are taken from the Northeastern University School of Nursing Virtual Summer Academy 2020 Presentation on Temperature Assessment by Dr. Marybeth Pompei, Senior Vice President and Chief Clinical Scientist Exergen Corporation and Affiliate Professor at Northeastern. Questions were posed by the Dean of the School of Nursing, and answers and recommendations provided by Dr. Pompei, as an expert in this field.
Getting the Best Results
Questions & Answers on Temperature Screening
 What are the recommendations from authorities for temperature screenings to be done at home?
What are the recommendations from authorities for temperature screenings to be done at home?
 American Academy of Pediatrics (AAP) School Guidelines
American Academy of Pediatrics (AAP) School Guidelines
“Testing & temperature checks. The CDC currently does not recommend COVID testing of students and staff. Testing only shows whether a person is infected at that specific moment in time and may not be useful in preventing outbreaks in school communities. Taking students' temperatures at school may also not be feasible, but you can monitor your children's health at home and keep them out of school if they are not feeling well and have a fever. Schools should frequently remind students, teachers, and staff to stay home if they have a fever of 100.4 degrees F or greater or have any signs of illness.”
Check out this article on Returning to School During COVID-19
Centers for Disease Control and Prevention (CDC)
- “CDC does not currently recommend universal symptom screenings (screening all students grades K-12) be conducted by schools.
- Parents or caregivers should be strongly encouraged to monitor their children for signs of infectious illness every day.
- Students who are sick should not attend school in-person.”
Screening K-12 Students for Symptoms of COVID-19: Limitations and Considerations
Massachusetts Department of Elementary and Secondary Education
“Checking for symptoms each morning by families and caregivers is critical and will serve as the primary screening mechanism for COVID-19 symptoms.41 Schools should provide information to families in their primary language to support them in conducting this symptom check and families should not send their children to school if they exhibit COVID-19 symptoms. We will be providing a checklist of symptoms and other guides to districts and schools to help families and students.
*Screening procedures are not required at the point of entry to the school. However, school staff (as well as bus drivers) should observe students throughout the day and refer students who may be symptomatic to the school healthcare point of contact.
*As noted in previous guidance, temperature checks are not recommended as screening for all students due to the high likelihood of potential false positive and false negative results.”
 How do circadian rhythms impact temperatures and assessments of temperatures?
How do circadian rhythms impact temperatures and assessments of temperatures?

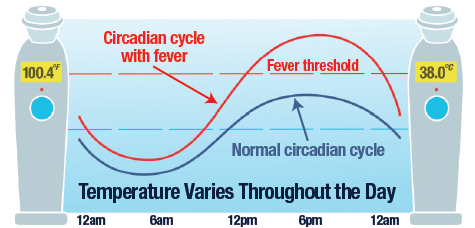 Our internal biological clocks produce circadian cycles that vary throughout the 24 hours of each day. This causes body temperature to vary about 1.6°F (0.9°C) between lowest temperatures in the morning and highest temperatures in the evening. With fever, the circadian variation still occurs, but at higher temperatures.
Our internal biological clocks produce circadian cycles that vary throughout the 24 hours of each day. This causes body temperature to vary about 1.6°F (0.9°C) between lowest temperatures in the morning and highest temperatures in the evening. With fever, the circadian variation still occurs, but at higher temperatures.
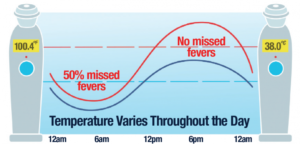 Accordingly, temperature assessments in the morning are low and will miss about half of the fevers. Temperature assessments in the evening are high and will detect all the fevers.
Accordingly, temperature assessments in the morning are low and will miss about half of the fevers. Temperature assessments in the evening are high and will detect all the fevers.
Mornings Not Ideal for Fever Screening. NYTimes/Reuters, May 27, 2020
“Morning fever screenings may be misleading. As businesses and cities reopen, screening people for fever when they arrive in the morning at work or school is likely to be widely used to help prevent coronavirus spread. But “morning may be the worst time” to screen for fevers, researchers say. They draw this conclusion from data collected from more than 300,000 people during studies of flu outbreaks in earlier years. “Fever-range temperatures… were rarest during mornings, and were about half as common during mornings as during evenings in periods of high influenza activity,” they report in a paper published on Tuesday without peer review on the medRxiv preprint server. “The results suggest that morning temperature measurements could miss many febrile disease cases,” they said.” (Read the Article)
Recent Published Studies on Circadian Effects on Fever
Harding et al (2020). Fevers Are Rarest in the Morning: Could We Be Missing Infectious Disease Cases by Screening for Fever Then? Undergoing peer review at https://doi.org/10.1101/2020.05.23.20093484
Harding et al (2020). Fever incidence Is Much Lower in the Morning than the Evening: Boston and US National Triage Data. West J Emerg Med. 2020 Jun 24;21(4):909-917. doi: 10.5811/westjem.2020.3.45215. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7390559/
Harding et al (2019). The daily, weekly, and seasonal cycles of body temperature analyzed at large scale. Chronobiol Int. 2019 Dec;36(12):1646-1657. doi: 10.1080/07420528.2019.1663863. Epub 2019 Sep 17. https://publishingimages.s3.amazonaws.com/eZineImages/PracticePerfect/706/The_daily_weekly_and_seasonal_cycles_of_body_temperature.pdf

 When do you recommend that temperatures be taken for school-aged youth?
When do you recommend that temperatures be taken for school-aged youth?

 Twice Daily. Before leaving for school in the morning, and at dinner time in the evening.
Twice Daily. Before leaving for school in the morning, and at dinner time in the evening.
If a fever is detected at either time, the student stays home and parents should contact their medical care professional immediately.
Even if the student is learning on-line, it is important to check temperature twice daily for the sake of the health of students and family members.
 .
. 
 What types of thermometers are recommended for use in schools? For use by families?
What types of thermometers are recommended for use in schools? For use by families?

 Only those that are clinically accurate as demonstrated by published peer-reviewed clinical studies.
Only those that are clinically accurate as demonstrated by published peer-reviewed clinical studies.
For school nurses checking students that might be sick, a professional grade fast, accurate, non-invasive thermometer scanning the temporal artery with more than 80 published peer-reviewed clinical studies, is best.
 For families, a home model thermometer that is fast, accurate, and non-invasive, scanning the temporal artery, backed by more than 80 published peer-reviewed clinical studies, is best.
For families, a home model thermometer that is fast, accurate, and non-invasive, scanning the temporal artery, backed by more than 80 published peer-reviewed clinical studies, is best.
 How is the cut-off for fever chosen?
How is the cut-off for fever chosen?
 100.4°F (38.0°C) is the medically accepted definition of a fever for more than 100 years.
100.4°F (38.0°C) is the medically accepted definition of a fever for more than 100 years.
This is recommended by AAP, CDC and WHO, and used in every medical institution in the world.
 Can you explain how a thermometer margin of error might guide the choice for a cut-off of fever?
Can you explain how a thermometer margin of error might guide the choice for a cut-off of fever?
 Some attempts to use a lower cut-off for Covid-19 screening have been made due to the low readings of the no touch thermometers from their inaccuracies.
Some attempts to use a lower cut-off for Covid-19 screening have been made due to the low readings of the no touch thermometers from their inaccuracies.
These attempts have been unsuccessful in “improving” the no touch devices’ accuracies. A thermometer with accuracy backed by more than 80 published peer reviewed studies requires no adjustment to the medical standard cut-off for fevers.
Exergen Twice Daily Resources
- Exergen Fever Guide.
- Accuracy backed by more than 100 peer-reviewed published studies. Read the Clinical Studies.
- Where to buy the Exergen Temporal Scanner Home Model.

Medical information disclaimer. This document may contain general information relating to various medical conditions and their treatment. Such information is provided for informational purposes only and is not meant to be a substitute for advice provided by a doctor or other qualified health care professional. Readers should not use the information contained herein for diagnosing a health or fitness problem or disease, and should always consult with a doctor or other health care professional for medical advice or information about diagnosis or treatment.